Understanding Surgery Options to Treat Diverticulitis
Diverticulosis disease is a very common condition that affects 20 percent of people by the time they reach the age of 40, and up to 70 percent of people over the age of 60.
It is diagnosed when small, bulging “pouches” are detected and become inflamed along the lining of a person’s digestive system. The good news is that the majority of people with this condition never develop symptoms. But when one of those pouches becomes blocked with hard stool, inflammation settles in and seeking care from a doctor who specializes in treatment of diverticulitis is important.
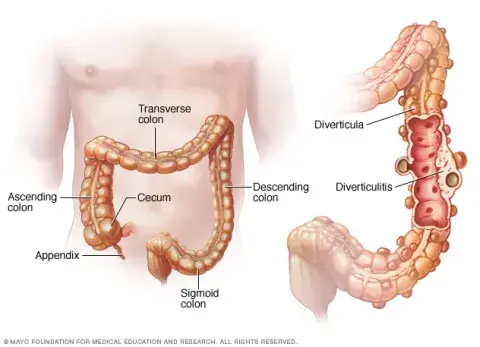
Patients with mild cases of diverticulitis may experience abdominal pain (usually on the left side of their stomach), constipation, and occasional fevers. In most instances, mild cases can be resolved with antibiotics, taken orally. More severe or complex cases of diverticulitis typically require a CT scan to assure an accurate diagnosis can be made and the proper plan of care can be created, which could include IV antibiotics administered in the hospital, drainage of an abscess, and in some cases, surgery.
Surgery for patients diagnosed with diverticulitis is classified as urgent, semi-urgent, or elective:
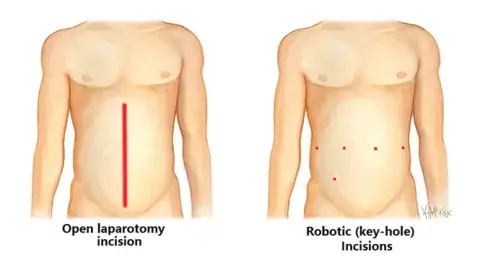
Urgent cases are performed when the pouches on the colon have ruptured and resulted in infection, spread across the abdomen. These cases are often necessary in order to save the life of the patient and involve removal of the ruptured area and placement of a colostomy (stool bag). This type of surgery is typically performed using a traditional “open” incision but not always.
Semi-urgent surgical cases are typically scheduled when a patient with acute diverticulitis is seeing no improvement after taking antibiotics and allowing for bowel rest. In these cases, the affected portion of the colon is removed, and during the surgery a decision is made on whether or not the patient requires a colostomy. These surgeries can be performed using a traditional “open” incision or minimally invasive techniques.
Elective surgery for diverticulitis is typically considered when a patient is experiencing symptoms with increasing frequency. Chronic diverticulitis is when the bowel becomes stiff and cannot process large amounts of roughage or fiber, and the patient may experience discomfort frequently after meals. Patients who elect to undergo surgery in these situations are almost always operated on using minimally invasive approaches – either laparoscopic or robotic techniques. The patient’s age and overall health must be considered in determining if surgery is an ideal treatment pathway when diverticulitis is deemed chronic but not life-threatening.
Clinical care providers at Beebe are committed to promoting lifestyle choices and changes that can prevent the development of diverticulitis. We recommend a diet rich in fibers and fluids, in order to minimize risk. We also educate patients about the signs and symptoms of diverticulitis, and how a screening colonoscopy can detect it early. Routine colonoscopies are designed to detect polyps and cancers of the colon. Screenings are recommended for people once they reach the age of 45 (or earlier for high-risk individuals).




